Table of Contents
- Emerging Trends in Health Policy Shaping the Future of Care
- Understanding the Impact of Legislation on Public Health Outcomes
- Innovative Strategies for Improving Access to Healthcare Services
- Navigating the Challenges of Health Policy Implementation
- The Importance of Stakeholder Engagement in Shaping Effective Health Policies
- Q&A
- The Way Forward
Emerging Trends in Health Policy Shaping the Future of Care
The landscape of healthcare is undergoing a seismic shift, driven by a variety of emerging trends in policy-making that will undoubtedly shape future care systems. One such trend is the increased focus on health equity. Policymakers are becoming more aware of the disparities in healthcare access and outcomes influenced by socio-economic factors. As a result, initiatives aimed at addressing these inequalities are gaining traction, fostering collaboration among various stakeholders to implement targeted interventions.
This commitment to health equity can manifest through programs that allocate funding to underserved communities, encouraging the development of clinics and preventive care services tailored to specific populations. Additionally, legislation aimed at dismantling systemic barriers is becoming a priority, aiming to create a more inclusive and fair healthcare system for all.
Another noteworthy trend is the integration of technology in health policy. The rapid advancement of digital health tools has prompted a reevaluation of how care is delivered. Telehealth, for example, has transitioned from being a temporary solution during the pandemic to a staple in many healthcare strategies. Policies are now evolving to support the reimbursement and regulation of telemedicine services, ensuring that quality care remains accessible regardless of geographic constraints.
Furthermore, there is a significant push for the incorporation of health data analytics to enhance decision-making processes within healthcare systems. By leveraging big data, healthcare providers can personalize treatment plans and improve patient outcomes more efficiently.
Lastly, the growing emphasis on mental health in policy discussions cannot be overlooked. As societal stigma continues to diminish, mental health services are being integrated alongside traditional healthcare offerings. This shift acknowledges that mental and physical health are interlinked, prompting comprehensive care approaches that address both realms together.
Legislative frameworks are now being designed to improve accessibility to mental health resources, allowing for better funding for programs that provide preventative care, crisis intervention, and long-term support. By prioritizing mental health, policymakers are taking essential steps towards building a holistic system that truly reflects the needs of the population.


Understanding the Impact of Legislation on Public Health Outcomes
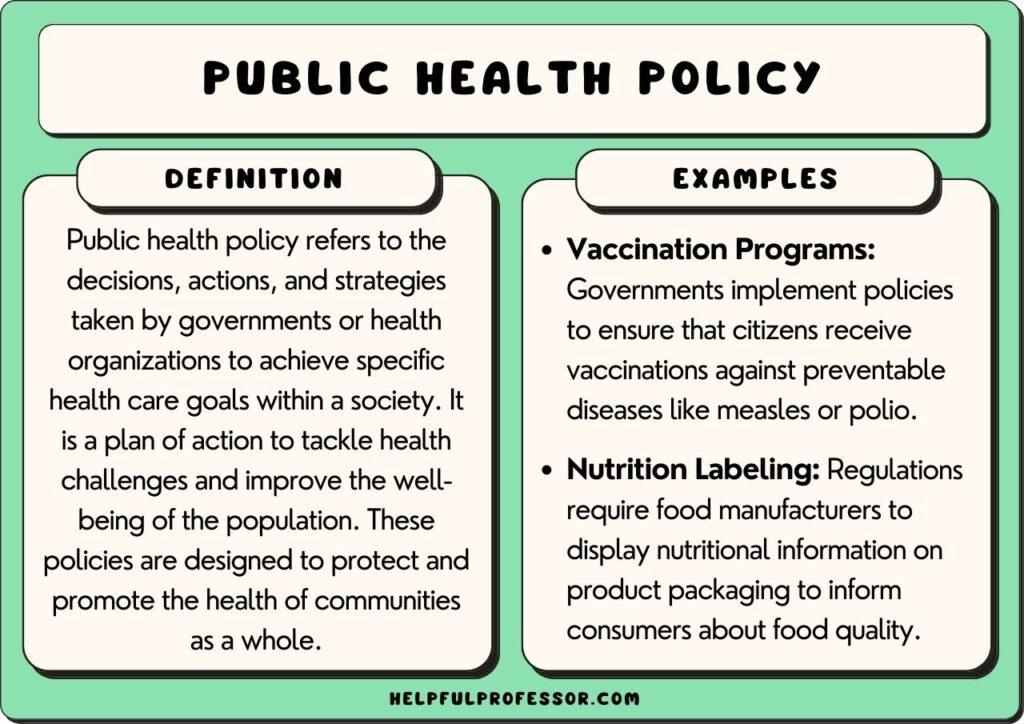
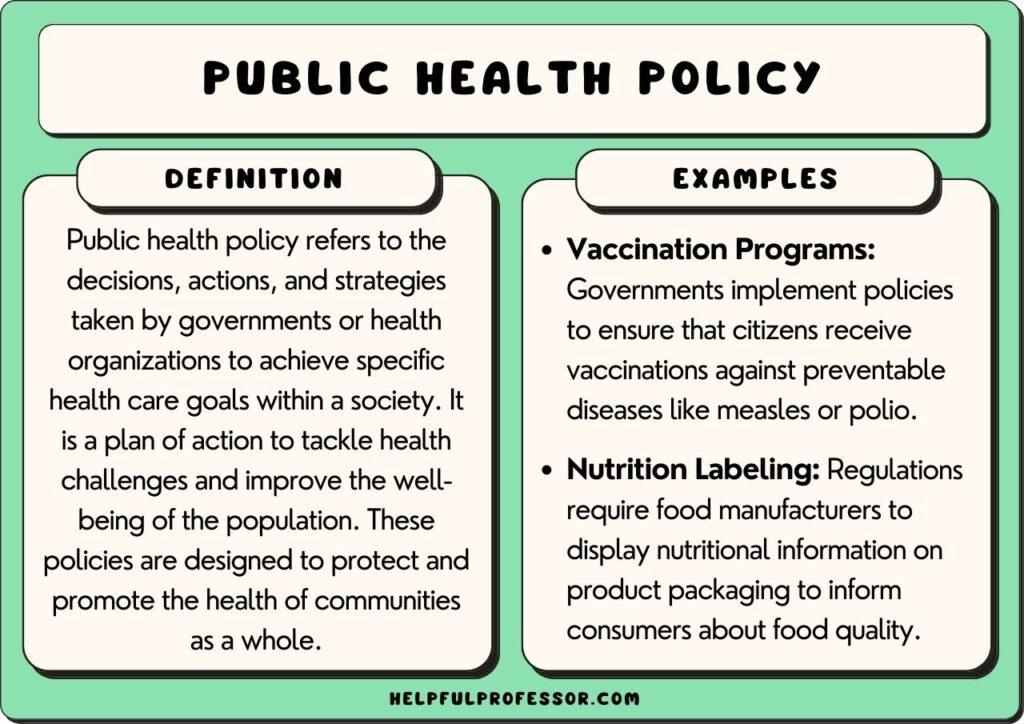
The connection between legislation and public health outcomes is profound. Legislative measures can shape health systems and influence the accessibility and quality of healthcare services. For instance, policies regulating air quality can significantly reduce respiratory diseases in urban populations. Similarly, laws mandating vaccination can lead to higher immunization rates, which directly impacts herd immunity and public health stability. The ripple effect of such legislation can be observed in various health metrics, illustrating the long-term benefits of proactive policy-making.
Moreover, legislation can address social determinants of health, which are crucial for overall well-being. Laws governing minimum wage, housing conditions, and education can indirectly influence health outcomes by altering socioeconomic factors. Communities with stronger economic protections tend to exhibit lower rates of chronic illnesses such as diabetes and hypertension. This demonstrates that public health policy isn’t confined to healthcare measures alone; it encompasses a broad spectrum of societal elements that ultimately shape individuals’ health experiences.
To illustrate the impact of legislation on public health outcomes, consider the following table showcasing some key health policies and their associated effects:
| Legislation | Health Impact |
|---|---|
| Affordable Care Act | Expanded healthcare coverage, reduced uninsured rates. |
| Tobacco Control Policies | Decreased smoking rates, lower incidence of lung cancer. |
| Safe Drinking Water Act | Improved access to clean water, reduced waterborne diseases. |
understanding how legislation affects public health is essential for advocating for more effective health policies. Engaging stakeholders from various sectors—including health professionals, policymakers, and community members—can lead to more comprehensive legislation that addresses both immediate health needs and long-term determinants of wellness.


Innovative Strategies for Improving Access to Healthcare Services
In the pursuit of enhancing healthcare accessibility, many organizations are piloting innovative frameworks that prioritize the patient experience. One compelling approach involves integrating telehealth services into existing healthcare structures, allowing patients to receive medical attention from the comfort of their homes. This shift not only reduces barriers such as transportation and long wait times but also expands the reach of specialists to underserved areas. By leveraging technology, healthcare providers can offer timely consultations and continuous care, alleviating pressure on physical facilities.
Community health initiatives represent another formidable strategy in the fight for better healthcare access. These initiatives focus on outreach and education, ensuring that local populations are aware of available services and how to utilize them effectively. Programs like mobile health clinics can be deployed in rural or marginalized urban neighborhoods, delivering primary care, vaccinations, and screenings directly to those in need. Furthermore, partnering with local organizations helps tailor services to culturally specific health issues, fostering trust and encouraging participation in preventive healthcare measures.
Lastly, incentivizing healthcare professionals through loan repayment programs and scholarships significantly boosts the availability of practitioners in high-need areas. By alleviating the financial burden of education, these programs attract more professionals to enter fields like primary care and pediatrics in underserved regions. Additionally, offering teleworking options can help retain talent by promoting work-life balance, helping to ensure that once healthcare professionals are in place, they remain committed to serving their communities effectively.
Navigating the Challenges of Health Policy Implementation
Health policy implementation is fraught with a variety of challenges that require careful navigation. Policymakers must engage with multiple stakeholders, including government entities, healthcare providers, and the communities they serve. Each of these groups brings a unique perspective, which can sometimes lead to conflicting priorities. For successful implementation, it is crucial to establish clear communication channels and foster collaboration among these parties. Regular meetings, feedback loops, and collaborative platforms can greatly enhance the transparency and trust needed for effective policy rollout.
Another significant obstacle lies in the allocation of resources. Funding limitations often restrict the ability to implement policy initiatives fully. Compounding this issue, the healthcare sector must respond to changing needs due to advances in technology, demographic shifts, and emerging health threats. To address these constraints, it is vital for policymakers to conduct cost-benefit analyses and prioritize initiatives that offer the most substantial impact. This approach enables decision-makers to allocate resources effectively while minimizing waste and maximizing outcomes.
| Challenge | Impact | Solution |
|---|---|---|
| Stakeholder Disagreement | Hinders progress and implementation | Establish clear communication and collaboration |
| Resource Allocation | Limits policy scope and effectiveness | Conduct cost-benefit analyses for prioritization |
| Changing Needs | Outdated policies | Continuous evaluation and adaptation of strategies |
Furthermore, ongoing evaluation and adaptation of health policies are critical in a dynamic healthcare environment. Monitoring the implementation process enables stakeholders to identify potential gaps in effectiveness early on. This responsiveness not only enhances the policies in practice but also ensures that adjustments can be made to meet emerging health needs promptly. By creating a culture of continuous improvement, health policy implementation can evolve, ensuring long-term success in delivering intended benefits to the community.


The Importance of Stakeholder Engagement in Shaping Effective Health Policies
Engaging stakeholders in the health policy-making process is crucial for developing policies that are not only effective but also equitable. Stakeholder engagement ensures that diverse perspectives are represented, leading to a more comprehensive understanding of the issues at hand. Health professionals, community members, and advocacy groups can provide vital insights that influence policy decisions. By fostering open dialogue and collaboration, policymakers can better align strategies with the real needs of the community, minimizing the risk of unintended consequences.
Furthermore, the transparency brought about by stakeholder involvement builds trust among the community and the policymakers. When stakeholders are included in discussions, they feel a sense of ownership over health initiatives. This ownership often translates into greater acceptance and adherence to health policies. Some key stakeholder benefits include:
- Enhanced collaboration between different organizations and sectors
- Informed decision-making based on localized data and context
- Increased buy-in from the community, leading to better health outcomes
Incorporating stakeholder input can also create opportunities for innovation. Policies shaped by collective insights often yield creative solutions that traditional approaches may overlook. A table highlighting the different categories of stakeholders and their contributions can illustrate this dynamic effectively:
| Stakeholder Category | Potential Contributions |
|---|---|
| Government | Policy formulation, funding allocation |
| Healthcare Providers | Clinical insights, patient care perspectives |
| Patients and Families | Personal experiences, community health needs |
| Nonprofits and Advocacy Organizations | Public health education, outreach strategies |
Ultimately, the engagement of stakeholders not only enriches the health policies being developed but also serves to empower the very communities that these policies are designed to serve. The collective input can lead to innovative strategies that prioritize health equity and ultimately result in improved public health outcomes.
Q&A
Q&A: Understanding Health Policy News Q1: What is health policy news, and why is it important? A1: Health policy news encompasses developments, changes, and updates related to laws, regulations, and initiatives that affect public health and healthcare systems. Staying informed on health policy is crucial as it directly impacts access to medical services, healthcare costs, and the overall quality of care individuals receive. Consuming this news helps citizens understand how policies influence their health and well-being.Q2: What are some current trends in health policy that readers should be aware of? A2: Some key trends include the push for universal healthcare coverage, the ongoing debates around mental health services access, and the impact of technology on healthcare delivery, such as telemedicine regulations. Additionally, there is increased focus on health equity, addressing disparities among different populations, and the implications of public health emergencies like pandemics.
Q3: How can individuals stay updated on health policy news? A3: Individuals can keep abreast of health policy changes by subscribing to reputable news outlets that specialize in healthcare reporting, following public health organizations on social media, and joining newsletters from agencies like the World Health Organization (WHO) or the Centers for Disease Control and Prevention (CDC). Engaging in community health forums or discussions can also provide valuable insights.
Q4: Are there specific health policies currently under discussion that could significantly affect people’s lives? A4: Yes, several significant health policy issues are under discussion. For instance, legislation regarding prescription drug pricing reform aims to lower out-of-pocket costs for patients. Another important topic is the potential expansion of Medicare benefits, which could facilitate access to critical services for older adults. Each of these topics has the potential to affect millions of lives.
Q5: How do political changes influence health policy? A5: Political changes, such as shifts in administration or legislative control, can dramatically alter health policy direction. Different political ideologies influence priorities like funding for public health programs, healthcare affordability, and regulatory frameworks. For example, a government focused on expansion might pursue universal health coverage, while another may focus on reducing government involvement in healthcare.
Q6: Why should we care about local health policy news, as it sometimes seems overshadowed by national issues? A6: Local health policies play a vital role in determining the quality and accessibility of healthcare within communities. Local governments often implement initiatives addressing specific regional health challenges, such as access to clean water or tackling obesity rates through new programs. Awareness of local health policy fosters community engagement and enables residents to advocate effectively for their health needs.
Q7: What role do advocacy groups play in shaping health policy? A7: Advocacy groups are crucial in raising awareness about specific health issues, mobilizing public support, and influencing policymakers. They often conduct research, provide resources, and collaborate with stakeholders to promote policies that align with their goals. Through lobbying efforts, education campaigns, and grassroots movements, these organizations help ensure that diverse perspectives are represented in health policy discussions.
Q8: How can changes in health policy affect health outcomes in the long term? A8: Long-term health outcomes can be significantly influenced by changes in health policy. For instance, policies that improve healthcare access lead to early detection of diseases, better management of chronic conditions, and overall improved population health. Conversely, restrictive policies may lead to worsened health outcomes and increased healthcare disparities, underscoring the importance of thoughtful policy development and implementation.
By staying informed about health policy news, individuals can better advocate for their needs and contribute to conversations that shape the future of healthcare in their communities.




0 Comments